[Adobe Stock]
Obesity is a risk factor for many diseases, from diabetes to heart disease to Alzheimer’s disease (AD). While researchers have long suspected a link between insulin resistance and Alzheimer’s, giving rise to the research term type 3 diabetes (not a clinical diagnosis), the epidemiologic signal appears to be strongest for midlife obesity and insulin resistance. A new study from Houston Methodist reports mechanistic evidence for a plausible fat-to-brain pathway. The study, published in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, found that adipose-derived extracellular vesicles, cell-to-cell messengers, can accelerate amyloid-ꞵ aggregation in experimental models. Amyloid-β plaques are a hallmark of AD.
The researchers found that the lipid cargo of the extracellular vesicles is different for obese individuals, and that the presence and abundance of certain lipids changed how quickly amyloid-ꞵ built up in laboratory models. The team used mouse models and human body fat samples to study the vesicles and how to disrupt their communication.
How obesity has been linked to AD
According to the Alzheimer’s Society, obesity between the ages of 35-65 can increase dementia risk later in life by approximately 30%. Human brains shrink as they age, and research has shown that higher BMI is associated with smaller brain volumes and lower cortical thickness. Additionally, obesity can decrease resilience to the disease and cause inflammation, which is linked to dementia. In the U.S., obesity affects approximately 40% of the U.S. population, and AD affects more than 7 million people.
Previous studies have shown that cohort studies link dyslipidemia with dementia risk; evidence on risk reduction via lipid-lowering remains mixed. Other mechanisms associated with the disease include lipotoxicity, insulin resistance, adipokine signaling, inflammation and immune cell fate shifts; all of which are more common and severe in individuals with obesity.
Lipid metabolism influences multiple processes in AD, including neuronal damage. Studies have shown changes in the levels of lipid classes in early-stage AD brains.
The team stated that future work should focus on how drug therapy could stop or slow the build-up of AD-associated proteins in at-risk individuals.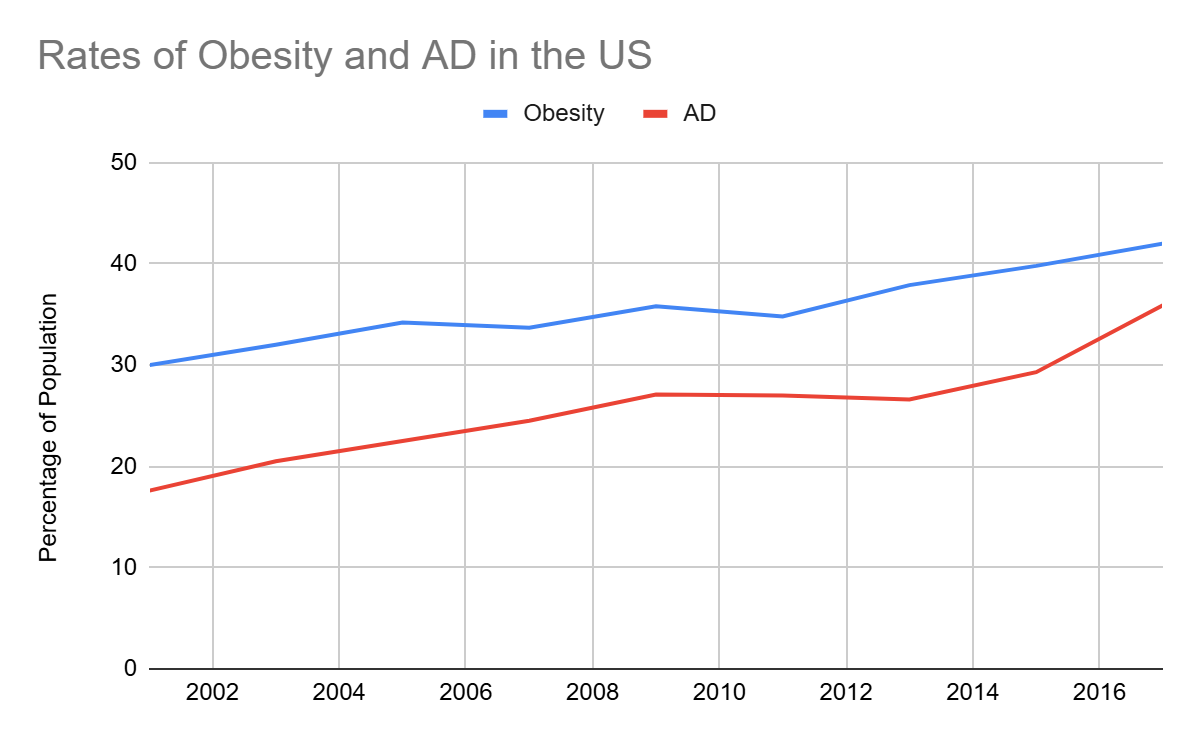
Read the full article from the Source